 Celiac disease is an autoimmune disorder impacting the small intestine, stemming from an abnormal immune response to gluten – a protein present in wheat, barley, and rye. This chronic condition, often misconstrued, exerts a profound influence on an individual’s well-being, necessitating meticulous management through adherence to a gluten-free lifestyle.
Celiac disease is an autoimmune disorder impacting the small intestine, stemming from an abnormal immune response to gluten – a protein present in wheat, barley, and rye. This chronic condition, often misconstrued, exerts a profound influence on an individual’s well-being, necessitating meticulous management through adherence to a gluten-free lifestyle.
Understanding the Basics of Celiac Disease
Celiac disease transcends the realm of food allergies or intolerances; it stands as a distinctive autoimmune condition. The small intestine lining is attacked by the immune system of people with celiac disease when they eat gluten-containing foods. Over time, this immune response damages the small intestine, resulting in a variety of symptoms and possibly long-term health issues.
Symptoms and Their Manifestations
The symptoms associated with celiac disease exhibit considerable variation, posing a challenge to accurate diagnosis. Common manifestations include abdominal pain, diarrhea, fatigue, weight loss, and bloating. However, non-digestive symptoms such as joint pain, headaches, and skin rashes can also be prevalent. In children, celiac disease may impede growth and development.
Diagnosis
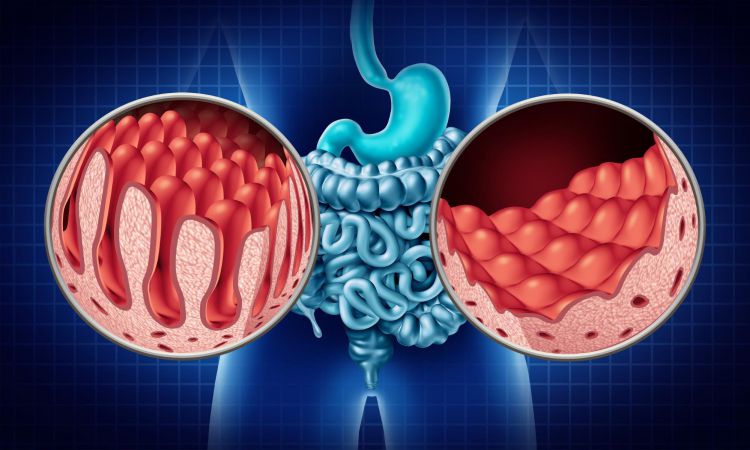
Diagnosing celiac disease involves a comprehensive approach, encompassing medical history, physical examinations, blood tests, and a definitive confirmation through a biopsy of the small intestine. A celiac disease test assesses the levels of specific antibodies linked to celiac disease, while a biopsy provides visual confirmation of the damage to the intestinal lining.
The Genetic Component
Celiac disease exhibits a robust genetic component. Individuals with a first-degree relative (parent, sibling, or child) diagnosed with celiac disease face an elevated risk of developing the condition. However, genetic predisposition alone does not suffice for the disease to manifest; exposure to gluten is an indispensable factor.
Treatment
The primary and sole effective treatment for celiac disease resides in a stringent gluten-free diet. This mandates the avoidance of all foods and products containing wheat, barley, and rye. Those with celiac disease must scrutinize food labels, exercise caution regarding cross-contamination, and opt for gluten-free alternatives. In certain instances, nutritional supplements may be recommended to address deficiencies arising from malabsorption.
Living Gluten-Free
Embracing a gluten-free lifestyle entails more than the exclusion of specific foods; it necessitates a significant shift in daily habits. This transition involves self-education on hidden sources of gluten, exploration of gluten-free recipes, and the discovery of alternative grains and flours. Negotiating social situations, dining out, and traveling while adhering to dietary restrictions comprise a learning curve in the gluten-free journey.
Potential Complications
Undiagnosed or untreated celiac disease can precipitate various complications, including malnutrition, osteoporosis, infertility, neurological disorders, and an elevated risk of certain cancers. Timely diagnosis and unwavering commitment to a gluten-free diet are pivotal in managing the condition and mitigating potential complications.
Gluten Sensitivity vs. Celiac Disease
It is imperative to draw a distinction between celiac disease and non-celiac gluten sensitivity (NCGS). While both conditions involve sensitivity to gluten, celiac disease is an autoimmune disorder with specific diagnostic criteria. In contrast, NCGS is a less clearly defined condition devoid of autoimmune processes but capable of causing similar symptoms.
Conclusion
Celiac disease emerges as a complex and multifaceted condition demanding meticulous management and a lifelong dedication to a gluten-free lifestyle. Beyond its physical ramifications, celiac disease can exert emotional and social implications, shaping how individuals interact with food and navigate various aspects of their lives. As awareness burgeons, education becomes paramount in dispelling myths and fostering understanding about celiac disease.
For those diagnosed, the journey encompasses symptom management, the embracement of a new relationship with food, and the discovery of a supportive community sharing similar experiences. Continued research and heightened awareness are propelling efforts to enhance the quality of life for those affected by celiac disease, paving the way for improved diagnostics and treatments.











